Ventilation for Pompe Disease – What You Need to Know
Patients with late-onset Pompe disease (LOPD) usually develop breathing problems as the disease progresses. If you have LOPD, you may eventually need ventilation to aid your breathing.
Here is more information about how Pompe affects breathing and about ventilators that may help to ease the disease’s symptoms.
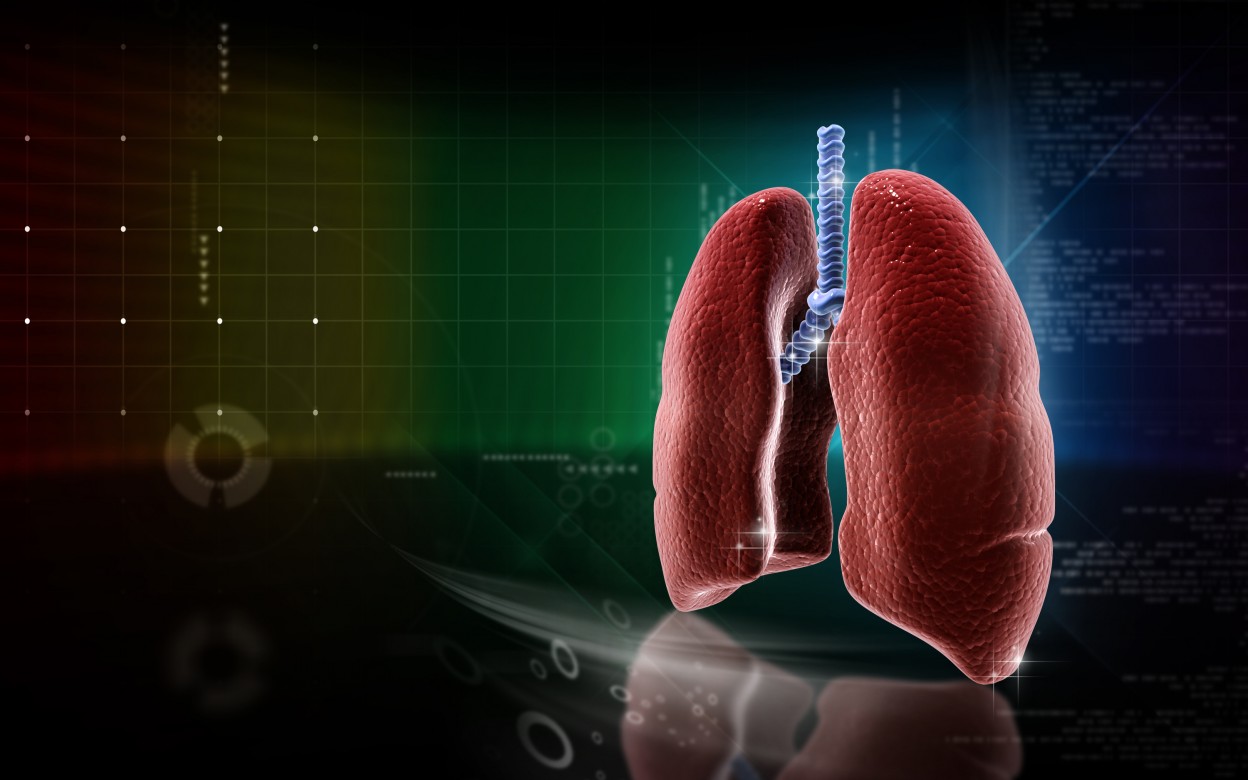
How does breathing normally work?
During normal breathing, the brain sends signals to the muscles in the body, which work together to either bring air into the lungs or exhale it out.
During inhalation, or breathing in, the large diaphragm muscle in the chest — situated below the lungs — contracts and moves away from the lungs. This movement creates more space in the chest and allows air to flow in. When breathing out, the diaphragm relaxes, pushing against the lungs and helping with exhalation.
Depending on the type of breathing, muscles around the ribs and abdomen may play a role in the process.
How does Pompe affect breathing?
In Pompe disease, mutations in the GAA gene cause the acid alpha-glucosidase enzyme to not function properly. The role of this enzyme is to break down glycogen — a stored form of the sugar glucose. So, if the enzyme does not work properly, glycogen builds up inside cells.
Muscles are typically one of the major storage sites for glycogen. However, in Pompe disease, glycogen levels are so high that they result in muscle damage and weakness. If the disease affects the diaphragm, breathing can become difficult.
If you have Pompe, you may eventually need ventilator support to breathe. Sometimes trouble breathing during sleep precedes a more general loss of breathing function. Researchers estimate that 75% of LOPD patients will eventually require ventilation.
In addition to the slow progressive loss of breathing function, patients with LOPD are at risk of acute respiratory failure due to lung infections. Patients may need shorter-term ventilation during these periods.
What is ventilation?
A ventilator is a machine that helps patients breathe. Most devices pump air into the lungs to aid in inspiration, or breathing in. Then, the machine pauses and allows patients to exhale on their own. If patients can’t exhale themselves, the ventilator also can assist with that function.
Main types of ventilation for Pompe
For patients with acute respiratory failure, non-invasive ventilation is typically used for short periods until the individual recovers from the illness. The ventilation in these systems is usually provided through a face mask that covers the patient’s nose, mouth, or both.
These non-invasive systems also may help in chronic respiratory failure cases, especially if the patient doesn’t need assistance all the time. Many individuals only need ventilation at night while they sleep.
For long-term respiratory assistance, patients will usually need a tracheostomy. This is a procedure that involves the creation of a small hole through the skin of the neck and into the trachea, or windpipe.
What happens once a patient is on a ventilator?
Being on a ventilator is often uncomfortable as the sensation of having air blown into the lungs can be unpleasant at first. It also can limit your mobility, although some portable ventilators are available. Depending on the system, it may be hard to talk or eat while using a ventilator. If you are not able to eat with your ventilator, you may need a feeding tube.
While using a ventilator, the tube may need to be suctioned to help keep it clear, especially if you have an infection. You may need special cough assistance devices to clear out phlegm and other airway secretions that can buildup in your lungs over time.
What are the risks of being on a ventilator?
One of the biggest risks of being on a ventilator is an infection, especially pneumonia, as the ventilator can potentially allow viruses and bacteria to get into your lungs.
Other risks include damage to the lungs or vocal cords, a buildup of fluid in the lungs, blood clots and skin irritation, and pneumothorax, or a buildup of air in the chest outside of the lungs. Atelectasis, a condition where the lungs might not fully inflate, is another possible risk of ventilation.
It is important for you to know the risks and to discuss with your physician how to best manage possible side effects. Ventilation can help you breathe better as Pompe disease progresses.
Last updated: Feb. 9, 2021
***
Pompe Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.