ERT for Late-onset Pompe Not Linked to Increased Risk of White Matter Lesions
Written by |
Aging and vascular risk factors, not enzyme replacement therapy or the disease itself, may increase the risk of late-onset Pompe disease patients developing white matter lesions in the brain, a study suggests.
The study, “White matter lesions in treated late onset Pompe disease are not different to matched controls,” was published in the journal Molecular Genetics and Metabolism.
Pompe disease is characterized by genetic mutations in the GAA gene, which lead to defective production of the alpha-glucosidase enzyme and consequent toxic accumulation of glycogen, a complex sugar molecule, in cells.
Enzyme replacement therapy (ERT) significantly improves survival and delays disability in patients with classic infantile-onset and late-onset Pompe disease.
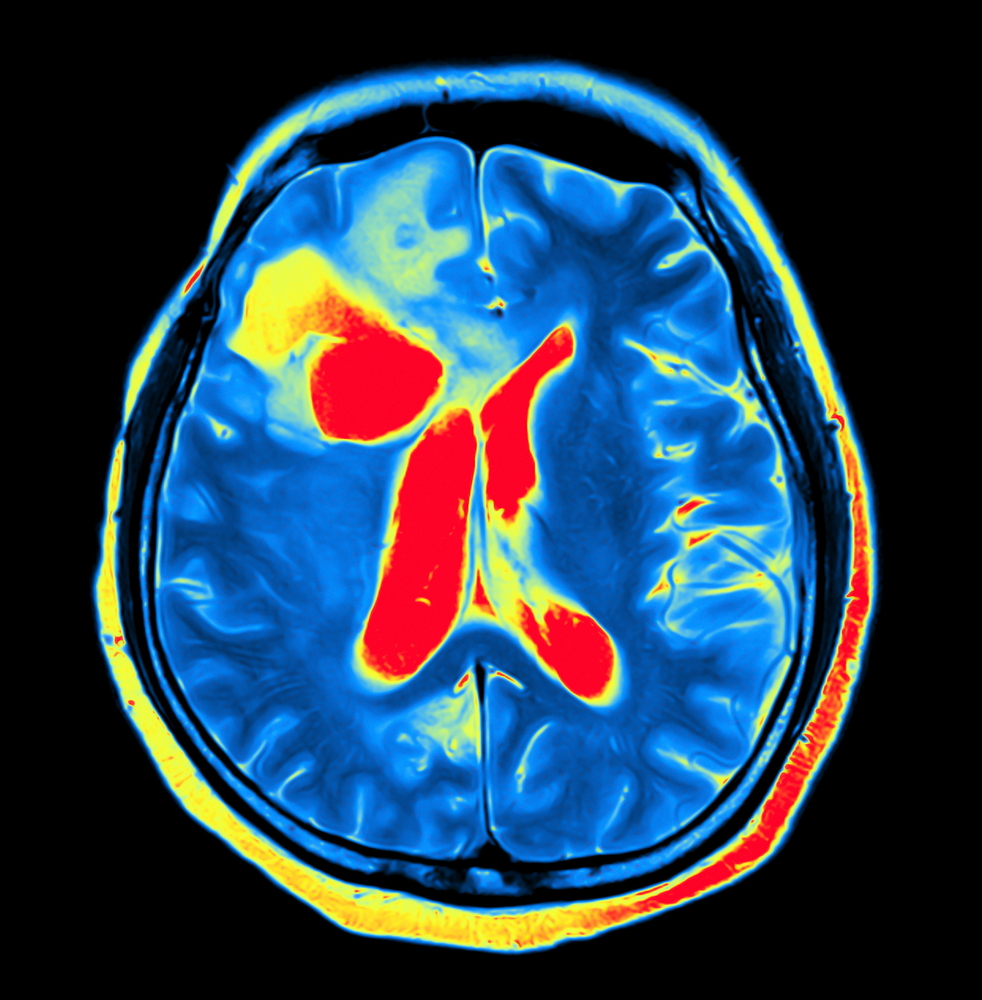
However, evidence suggests that in these patients, treatment with ERT is linked to the development of progressive white matter abnormalities. The white matter is made up of axons, the extensions in neurons, and is found in the deeper tissues of the brain and the outer tissues of the spinal cord. It is one of the two kinds of tissues in the central nervous system; the other one is grey matter.
In this study, researchers investigated the impact of disease and ERT on LOPD patients’ risk of developing white matter lesions.
They studied 19 LOPD patients (10 females, nine males), median age 54.4 years, undergoing regular ERT (median duration of the treatment was 63 months).
Researchers analyzed brain scans, performed using magnetic resonance imaging, to detect white matter abnormalities. They then compared the brain scans with those of 38 age- and sex-matched controls. Patients and controls were also matched for risk factors, including hypertension (high blood pressure), hyperlipidemia (high lipid or fat content in the blood), obesity, smoking, and diabetes.
The analysis detected white matter lesions in 63% of the LOPD patients (12 of 19) and in 66% (25 of 38) controls. Researchers then scored the lesions using the Fazekas Score, which ranges from zero to three, and where increasing scores mean more and larger lesions.
Researchers found no differences in the Fazekas Score between LOPD patients and matched controls — the mean total of Fazekas score in LOPD was 2.42; in the controls, 1.60. The volume of the white matter lesions was also similar between LOPD patients (mean 5.27 ml) and controls (7.89 ml).
The total Fazekas Score correlated with participant age in both LOPD patients and controls. Moreover, the researchers saw that longer treatment with ERT was linked with a lower score, suggestive of a “somehow protective influence of ERT.”
Overall, these findings suggest that white matter lesions “in LOPD mainly result from concomitant cerebrovascular risk factors rather than from the Pompe disease itself,” the study concluded.


