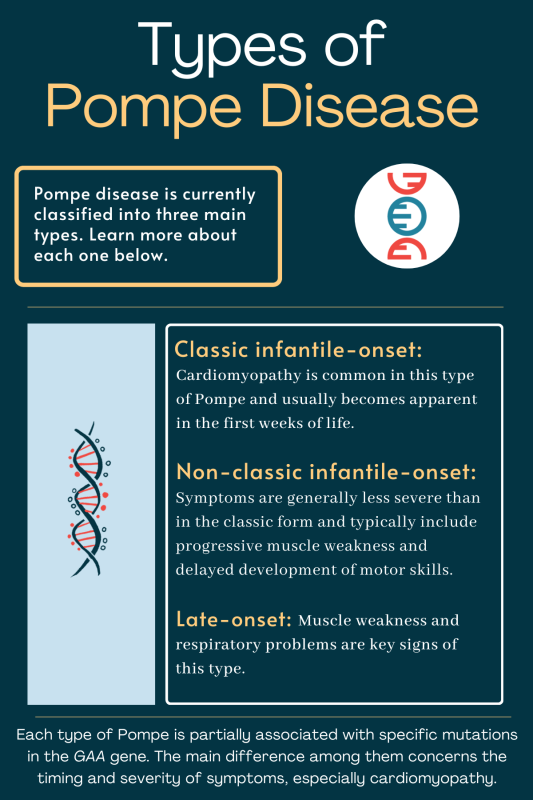
FAQs about types of Pompe disease
In general, earlier age at onset is associated with more severe, faster-progressing symptoms in Pompe disease. Consequently, the late-onset form — also referred to as juvenile/adult-onset — is typically considered the mildest type of Pompe disease.
The most common type of Pompe disease is the classic infantile-onset form.
Pompe is a progressive disease. The symptoms of the genetic disorder are caused by a complex sugar molecule, called glycogen, building up to toxic levels inside cells. This is due to deficiencies in the cellular machinery that usually break it down. The symptoms of Pompe will continually get worse as glycogen builds to even more toxic levels in cells over time.
When a person breathes, a number of muscles are involved in sucking air into the lungs and pushing it back out again. These muscles may be affected in Pompe, resulting in respiratory problems. Such problems may develop in all types of Pompe disease, though they are generally more severe in infantile-onset forms.
Yes, Pompe disease is considered both a lysosomal and a glycogen storage disorder. Lysosomes are cellular compartments that act as the cell’s “recycling centers,” breaking down complex molecules into simple components. Lysosomal storage disorders are a group of genetic conditions in which specialized proteins (enzymes) don’t work correctly, leading to a toxic buildup of complex molecules that would normally get broken down in the lysosome. The GAA enzyme, the deficit of which causes Pompe disease, is a lysosomal protein that helps to break down a complex molecule called glycogen. Because it affects the lysosomes, Pompe is considered a lysosomal storage disorder. Pompe also is considered a glycogen storage disorder because it specifically leads to a buildup of glycogen in cells.
Related Articles

 Fact-checked by
Fact-checked by