FAQs about Pompe disease symptoms
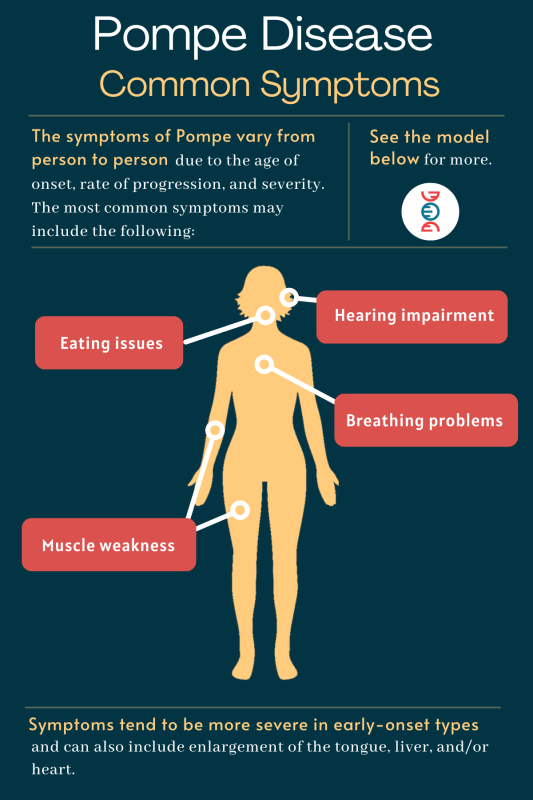
Across the different types of Pompe disease, nearly all patients experience muscle weakness. Breathing problems and difficulty eating also are common in people with a Pompe disease diagnosis. Almost all babies with the classic infantile-onset form of the disease develop an enlarged heart and heart disease.
Pompe disease causes are linked to genetic mutations that render the body unable to break down glycogen, a complex sugar molecule used by some cells as a form of short-term energy storage. Muscle cells, which require a lot of energy to power movement, normally store significant amounts of glycogen, thus muscles are primarily affected in Pompe. Cells of the heart and skeletal muscles (muscles responsible for the movement of body parts) are the most affected.
When a person breathes, muscles in the diaphragm work to push air into and out of the lungs. Pompe disease can cause weakness in these muscles, and likely also in other accessory respiratory muscles, which can lead to impaired breathing.
The speed of Pompe progression varies widely from person to person, depending on the type of disease as well as treatments and other factors. In general, an earlier onset of symptoms is associated with a faster disease progression.
Every person inherits two copies of the GAA gene, one from each biological parent. Pompe will only develop if both copies of this gene contain a disease-causing mutation. Carriers, who have only one mutated copy (and one healthy copy), will not develop Pompe symptoms, but they may pass the disease-causing mutation to their biological children.
Related Articles

 Fact-checked by
Fact-checked by