Phrenic nerve dysfunction tied to LOPD breathing issues in study
Findings may point to need for therapies that access spinal cord
Dysfunction of the phrenic nerve, which is important for controlling breathing, was observed in a small study of late-onset Pompe disease (LOPD) patients who had ongoing respiratory dysfunction despite enzyme replacement therapy (ERT).
“Our study provide new insights regarding respiratory mechanisms in LOPD,” the researchers wrote. Should their findings be validated, the design of new therapies that more easily access the spinal cord where the phrenic nerve resides are warranted, they said.
The study, “Diaphragm weakness in late-onset Pompe disease: A complex interplay between lower motor neuron and muscle fibre degeneration,” was published as a short communication in the Journal of Neurological Sciences. It was funded by Sanofi.
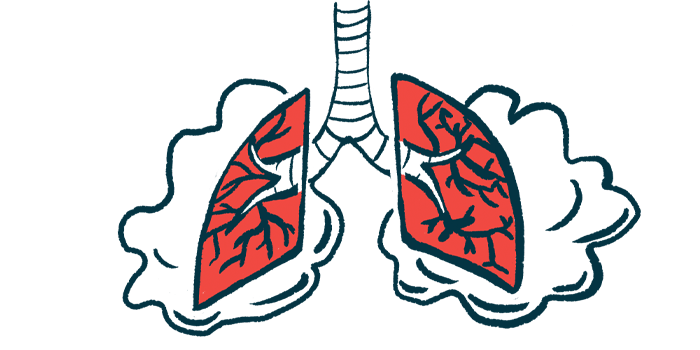
In LOPD, the harmful buildup of a large sugar molecule called glycogen in cells leads to slowly progressing muscle weakness, including weakness in the muscles needed for breathing. That happens because the enzyme that breaks glycogen down, alpha-glucosidase (GAA), is lacking due to genetic mutations. ERT provides a working GAA enzyme, helping to prevent glycogen accumulation, slowing declines in muscle strength, and preserving breathing functions.
For many, breathing problems persist despite ERT
Still, many patients continue to have breathing problems and rely on respiratory support at some point despite using ERT. The mechanisms underlying this persistent breathing dysfunction have yet to be understood, according to the researchers.
Muscle function is controlled by input from nerve cells. Signals from the phrenic nerve that runs through the spinal cord are what tell the diaphragm, the main breathing muscle, to expand and contract. Movement of the diaphragm is what allows the lungs to fill with or empty of air when inhaling and exhaling.
One theory is that abnormalities in the phrenic nerve could lead to diaphragm weakness that contributes to ongoing respiratory problems in LOPD.
To learn more, the scientists conducted studies to look at the health of the phrenic nerve in a group of eight symptomatic LOPD patients on ERT who were seen at their clinic in Portugal. Five relied on non-invasive ventilation support at night and were considered to have respiratory failure.
All participants underwent a nerve conduction study, which looks at electrical activity of a nerve in response to stimulation, to evaluate the phrenic nerve.
Phrenic nerve activity looked normal in the three patients without respiratory dysfunction, but the five who relied on respiratory support showed a loss of normal phrenic nerve activity.
Those five patients underwent further testing with electromyography, which is used to measure a muscle’s response when the nerve that controls it is stimulated. This can help doctors learn more about whether problems with nerve-muscle communication are coming from the nerve or the muscle.
For three patients, findings indicated problems in both the muscle itself (myopathic), as well as the nerves innervating them (neurogenic). Another person showed signs of myopathic changes only, and in another, no muscle signals could be measured at all, which the researchers said was “probably due to severe diaphragm affection.”
Overall, the “results support that spinal phrenic motor neurons dysfunction may contribute to respiratory failure,” the researchers wrote, noting that this is in line with earlier preclinical research.
The brain and spinal cord are protected by the selective blood-brain barrier, which prevents certain substances in circulation that could be harmful from reaching these important parts of the nervous system.
ERT does not readily cross this barrier, so any glycogen that’s accumulated near the phrenic nerve wouldn’t be effectively broken down by treatment, according to the researchers. Preclinical studies have shown that therapeutics designed to increase GAA could increase ventilation when delivered directly to the spinal canal.
“If confirmed in further studies, our results recommend the need of new drugs crossing the blood-brain barrier,” the researchers wrote.