Severe ERT under-treatment in LOPD tied to quality of life declines
Insufficient reimbursement is not uncommon, making reduced dose an option
Written by |
Late-onset Pompe disease (LOPD) patients who received severely under-dose treatment with enzyme replacement therapy (ERT) had a decline in physical quality of life, but an improvement in overall health, during a 14-month follow-up, a study in China shows.
Being employed or enrolled in school predicted improved mental quality of life, while female Pompe patients had a worsening of overall health during the study.
“A Pompe-disease specific instrument based on patient experiences is warranted to closely monitor changes in [quality of life] on a routine basis. It is desirable for patients with severe under-dose ERT to discuss with physicians whether to adjust treatment strategies,” the investigators wrote.
Their study, “Association between under-dose of enzyme replacement therapy and quality of life in adults with late-onset Pompe disease in China: A retrospective matched cohort study,” was published in PLOS One.
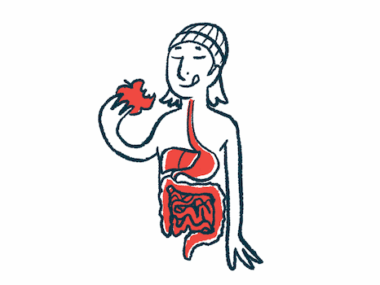
Pompe disease is caused by mutations in the gene that provides instructions for making the enzyme acid alpha-glucosidase, or GAA. Without GAA, a complex sugar molecule called glycogen builds up and damages cells, especially in the muscles and the heart.
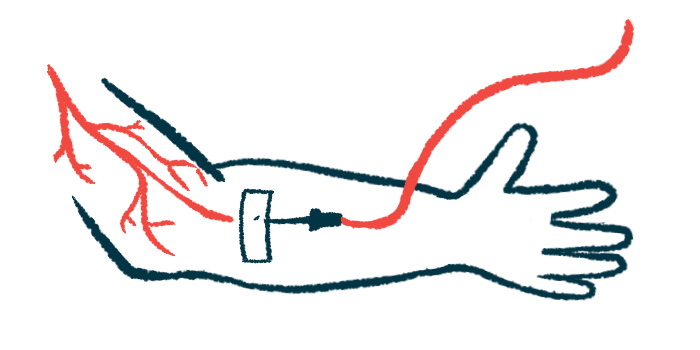
In LOPD, one type of the condition, symptoms develop at any point after the first year of life and typically manifests as progressive muscle weakness that especially affects the torso and legs. Breathing problems may also occur. ERT is a standard treatment strategy, wherein a therapeutic, lab-made GAA enzyme is infused into the bloodstream.
Effects of under-dose ERT
In China and other countries, insufficient ERT reimbursement is common, so reducing the dosage is given consideration to be able to afford ERT.
“In this patient-physician communication, under-dose use of ERT is a therapeutic decision under non-ideal conditions that physicians need to take account of the best interests of their patients, not only from a clinical perspective, but also from financial, emotional, and psychosocial perspectives,” wrote the researchers, who compared the effect of mild under-dose ERT for five people, severe under-dose ERT for six, and no ERT for 22 people on measures of quality of life, both mental and physical.
“Since few adult patients with LOPD used ERT with a standard dose in China, it is important to assess whether under-dose use of ERT could improve or stabilize health outcomes from a patient perspective compared with receiving no ERT,” the researchers wrote.
The ERT dose was measured as the reported ratio of actual vials used divided by the indicated vials patients should have used. All participants on ERT used the treatment with a ratio of vials lower than 70%. The five Pompe patients who used ERT above the median ratio were classified as mild under-dose users, while the six who used ERT below the median ratio were classified as severe under-dose users. Among the 33 participants, 81.8% said they depended on assistive devices, 21.2% used a wheelchair and 93.9% a ventilator to help with breathing.
Most (81.8%) participants with either mild or severe under-dose ERT had catastrophic health expenditure, defined as annual out-of-pocket health expenditures exceeding 10% of the family’s income. Aa smaller percentage (40.9%) not using ERT had catastrophic health expenditure.
Compared to the start of the study and to the group without ERT, severe under-dose ERT users had a significant decline in physical quality of life during follow-up, as assessed with the Short-Form Health Survey. But their subjective overall health state improved, as measured with the EuroQol 5-dimension instrument with a five-level scale, the benefit likely being “because these participants had hopes and expectations toward the therapy and felt healthier after receiving ERT,” the researchers said.
Being a female was a risk factor for a decline in overall health. Being employed or at school correlated with improvements in the mental health component of quality of life, “probably because patients who are employed or at school have more chances to interact with other people and perform better in their social roles,” wrote the scientists.
The classifications of mild under-dose and severe under-dose ERT users that relied at follow-up on participants’ self-reported number of vials used was called a study limitation because recall bias, or systematic errors that occur when participants don’t remember experiences accurately, may have happened.
“Customized interventions are needed to improve [quality of life] in vulnerable subgroups, including female and unemployed people,” the researchers wrote. “Future studies with a larger sample size and longer follow-up are warranted.”