How to build an LOPD care team that’s right for you
Last updated April 22, 2024, by Susie Strachan

When you work together with your care team to make informed decisions about managing late-onset Pompe disease (LOPD), it can help you feel more in control of this chronic condition.
Pompe disease is caused by mutations in the GAA gene. It leads to progressive muscle weakness. When Pompe disease symptoms develop at any point after 1 year of age, including in adulthood, it is called LOPD.
Along with approved treatments such as enzyme replacement therapy, a multidisciplinary healthcare team can provide coordinated care to treat LOPD symptoms, such as pulmonary, neuromuscular, orthopedic, and gastrointestinal issues.
Who is on an LOPD care team?
Multidisciplinary care for LOPD will help you get the guidance required to manage your condition.
The specific makeup of your LOPD healthcare team will depend on the symptoms you are experiencing and may change over time.
LOPD can cause a waddling or swaying gait and make it difficult to stand, run, or climb stairs. It also can cause a sideways curvature of the spine (scoliosis).
Typically, your primary care physician serves as your first point of contact. They can monitor your general health, do routine checkups, and offer referrals to specialists as needed.
In addition to your primary care physician, a number of LOPD specialists are commonly involved in managing this rare disease. They may include a pulmonologist, cardiologist, and neurologist. You also may require supportive therapy from physical, occupational, and speech therapists, along with registered dietitians.
The following specialists have expertise in different aspects of the condition to provide comprehensive care. They also can offer suggestions for living with Pompe disease.
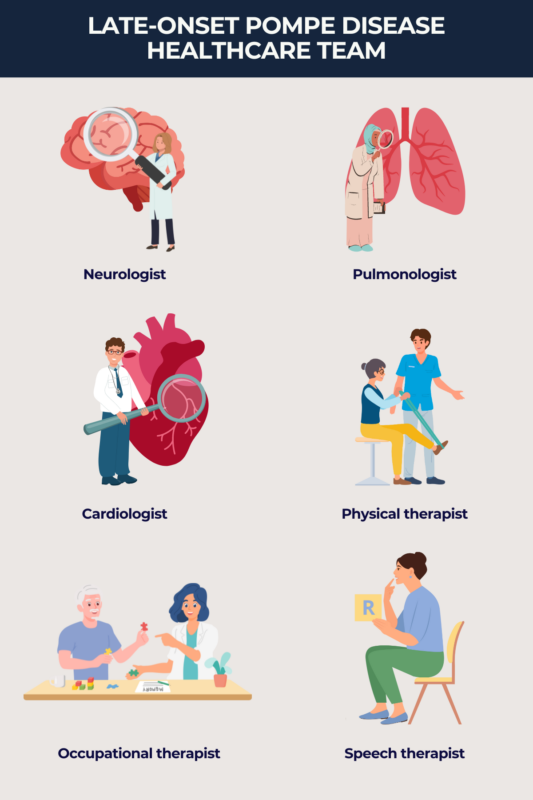
Pulmonologist
A pulmonologist specializes in diagnosing and treating conditions affecting the respiratory system.
LOPD care: A pulmonologist helps manage respiratory issues commonly associated with LOPD, such as breathing difficulties and respiratory muscle weakness that can affect your breathing.
What to expect: Pulmonologists may conduct pulmonary function tests and monitor lung function over time. They also may refer you to respiratory therapy to assess your overall ability to breathe as well as during specific situations, such as before starting an exercise program.
Cardiologist
A cardiologist focuses on diagnosing and treating heart conditions.
LOPD care: Cardiologists monitor heart health, assess cardiac function, and manage cardiovascular symptoms. Cardiac issues linked to LOPD include rhythm disturbances and an enlarged heart (cardiomegaly).
What to expect: Cardiologists may perform cardiac evaluations, such as an echocardiogram to detect abnormalities in the heart’s structure. An electrocardiogram is a test that shows how well your heart muscle is functioning and can detect an abnormal heart rhythm.
Neurologist
A neurologist specializes in disorders of the nervous system, including those affecting muscles and nerves.
LOPD care: Neurologists can assess and manage LOPD-related neurological symptoms such as muscle weakness, motor dysfunction, and peripheral neuropathy — nerve damage that can lead to numbness, tingling, pain, and weakness.
What to expect: A neurologist may order diagnostic tests such as an electromyogram to detect alterations in the electrical activity of your muscles or a muscle MRI to track muscle degradation from LOPD.
Physical therapist
Physical therapists focus on improving your mobility, strength, and ability to continue doing daily activities and tasks without assistance.
LOPD care: A physical therapist can develop a safe and effective exercise program that helps maintain or improve muscle function and addresses other related issues caused by LOPD, such as gait abnormalities.
What to expect: A physical therapist can show you exercises, along with guidance on assistive devices and techniques, to help mobility and reduce the risk of falls due to muscle weakness, pain, and fatigue.
Speech therapist
Speech therapists, also known as speech language pathologists, specialize in evaluating and treating communication and swallowing difficulties.
LOPD care: A speech therapist can help manage speech difficulties, swallowing problems (dysphagia), and related LOPD issues such as the risk of aspiration (food or liquid getting into your lungs).
What to expect: A speech therapist may work with you on strategies to improve communication, safe swallowing techniques, and ways to ensure you are getting adequate nutrition.
Occupational therapist
Occupational therapists specialize in helping you stay independent by improving your ability to perform daily tasks. They can suggest coping mechanisms such as following a daily routine.
LOPD care: An occupational therapist can help you maintain your independence and improve your quality of life by working with you on techniques for dressing, grooming, bathing, cooking, and household chores.
What to expect: An occupational therapist may make suggestions for modifications to your home to improve accessibility and safety. They also may assist you in learning how to use adaptive equipment for mobility, eating, and communicating.
Dietitian
A registered dietitian can do a comprehensive nutritional assessment to evaluate your diet, nutritional status, and metabolic needs.
LOPD care: A dietitian can assess how much energy you expend, your weight management goals, and take into account any gastrointestinal symptoms.
What to expect: A dietitian may recommend nutrient-dense foods that provide sustained energy, along with enough protein to support muscle repair and maintenance. Some people with LOPD may experience gastrointestinal symptoms such as bloating, constipation, or gastroesophageal reflux disease. The dietitian may recommend what foods to eat to avoid these issues.
Finding the right LOPD care team
To put together an LOPD care team, start by talking with your primary care physician about referrals to specialists who have experience in managing neuromuscular disorders such as LOPD.
Next, research healthcare providers and medical centers with expertise in diagnosing and treating LOPD. Look for centers of excellence or multidisciplinary clinics that specialize in neuromuscular disorders and offer comprehensive care for people with LOPD.
Professional organizations, patient advocacy groups, and LOPD support groups can provide information on healthcare providers and centers with experience in managing LOPD.
At your first appointment with a potential healthcare provider, ask questions about their experience with LOPD, approach to care, treatment philosophy, and communication style.
Remember, you are your own best advocate. Talk about your concerns and preferences, so your healthcare provider will hear what you need and work with you to develop a personal care plan.
The benefits of a coordinated approach
A coordinated care team can ensure all aspects of your health and well-being are addressed, from diagnosis and treatment to rehabilitation and ongoing LOPD management.
Each member of the care team brings their unique knowledge and skills to your LOPD treatment plan. Each team member should monitor your health and communicate any changes or complications to the other team members.
In addition to medical treatment, a coordinated approach includes support services such as physical therapy, occupational therapy, speech therapy, nutritional counseling, and mental health support. This holistic approach addresses your physical, emotional, and social needs, supporting overall well-being and quality of life.
Building a strong relationship with your care team
The goal of building a strong relationship with your LOPD care team is to receive the support, guidance, and personal care you need to effectively manage your condition.
Start by educating yourself about the disease and keeping up with the latest developments in research and treatment.
It’s also important to establish honest communication, by sharing your concerns, symptoms, preferences, and goals. This will help you understand and be able to consider the risks, benefits, and alternatives of different treatment options.
Do your best to stick with your treatment plan, such as taking prescribed medications and following dietary and lifestyle recommendations.
If you have concerns about your treatment plan, do not make changes on your own. First discuss them with your healthcare team.
Do not hesitate to give feedback to your healthcare team about your experiences with care, including what has helped you and what hasn’t. When you work together to make informed decisions about managing LOPD, it empowers you to take control of living with LOPD.
Pompe Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Related articles