Pompe Patients Have Abnormalities in Artery that Supplies Blood to the Brain, Study Shows
Written by |
Patients with Pompe disease may develop structural changes in the basilar artery — an important artery that supplies oxygen to the brain — that may affect their risk for cerebrovascular complications, such as stroke.
The study with that finding, “Decreased outlet angle of the superior cerebellar artery as indicator for dolichoectasia in late onset Pompe disease,” was published in the Orphanet Journal of Rare Diseases.
While Pompe disease is mainly characterized by muscular weakness and respiratory and cardiac insufficiency, patients also may develop complications in vessels that supply blood to the brain. These changes were previously reported to affect patients’ long-term survival, as they increased the risk for intracranial hemorrhages, compression of cranial nerves, and stroke.
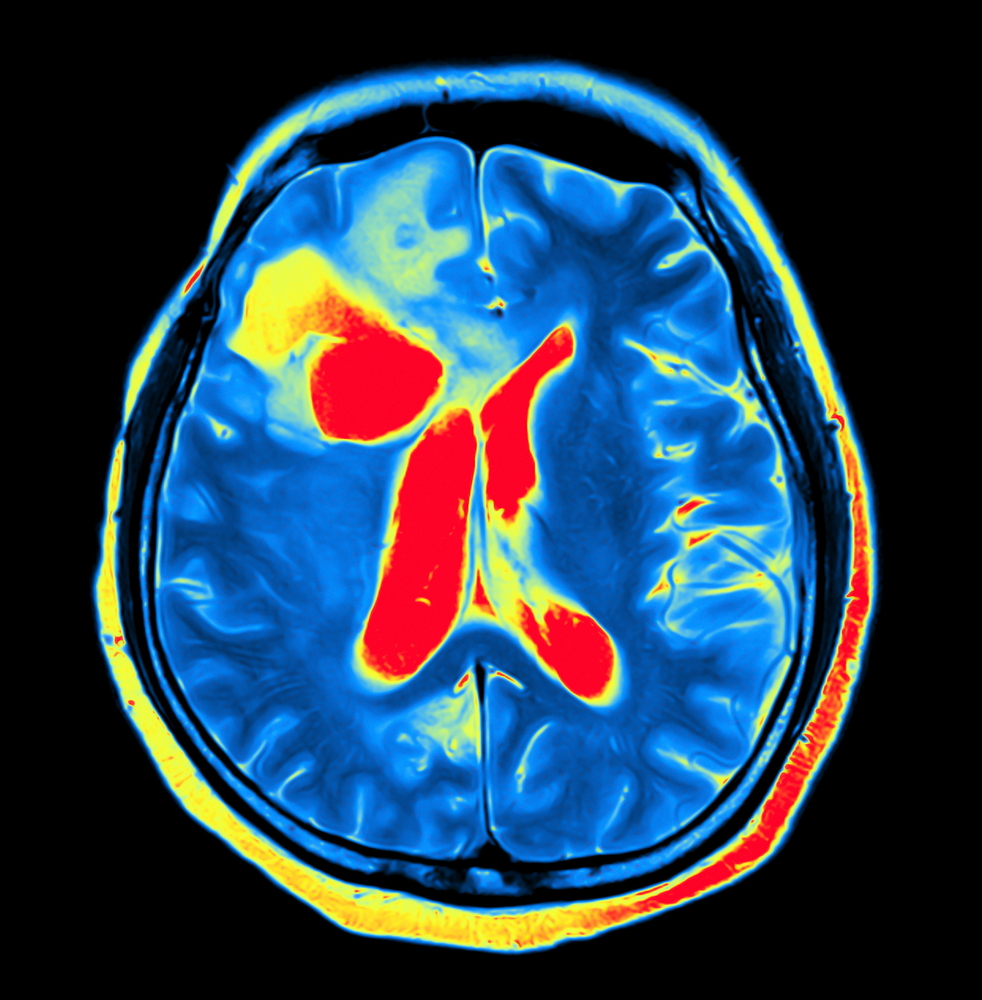
More recent studies have reported that the main blood vessel affected in the brain of Pompe disease patients is the basilar artery, which supplies oxygen-rich blood to some of the most critical parts of the brain. In Pompe patients, the artery can show signs of elongation, dilatation, and/or tortuosity, a condition known as dolichoectasia.
“However, little is known about the progression of this arterial remodelling in the course of LOPD [late onset Pompe disease],” researchers wrote.
They analysed the basilar artery’s length, diameter and volume, as well as brain lesions in 20 late onset Pompe disease patients, all undergoing enzyme replacement therapy (ERT), and compared it to 40 controls (patients with other neurological diseases) matched for age, sex, and cardiovascular risk factors. They looked particularly at the angle of the bifurcation of the basilar artery, thought to influence the risk and rupture of strokes.
About 4 percent of all ischemic strokes are caused by blockages in the basilar artery system.
The results showed that the height of the basilar artery bifurcation was abnormal in 60% of the Pompe patients and in 30% of the controls. Abnormal lateral displacement of the artery also was higher in Pompe disease relative to controls, 5% vs 2.5%, respectively.
The diameters of the middle and distal parts of the artery were significantly increased in Pompe disease compared to controls. Additional parameters that also changed in Pompe disease included the basilar artery’s length, volume and the outlet angle of the superior cerebellar artery (SUCA) from the basilar artery’s.
During a five-year follow up of nine Pompe disease patients, researchers saw that two of them developed an abnormal height of basilar artery bifurcation, and all of them had a reduction in the SUCA outlet angle.
During this period there were no major cerebrovascular events, with the exception of one patient – a 75-year-old woman experienced an intracranial hemorrhage on the left side that led to complete immobilization and subsequent death.
The patient was later shown to have the most prominent changes in its basilar artery that also affected the artery’s bifurcation.
White matter brain lesions occurred at similar rates in both groups, 63% and 68% in Pompe patients and controls, respectively.
In conclusion, researchers recommend that “patients without cerebrovascular abnormalities undergo a follow-up of MRI [magnetic resonance imaging] analysis after 5 years. In patients with cerebrovascular abnormalities, we recommend the strict treatment of cerebrovascular risk factors (e.g. hypertension) and follow-up imaging after 1 to 2 years.”


