Benefits seen for IOPD children switching to Nexviazyme: Study
Greater gains seen with ERT transition from Myozyme at younger age
Written by |
Children with infantile-onset Pompe disease (IOPD) experienced reductions in disease-related biomarkers and stabilizations or improvements in clinical function after switching from Myozyme (alglucosidase alfa) — sold as Lumizyme in the U.S. — to Nexviazyme (avalglucosidase alfa), according to a new study from Taiwan.
These functional improvements were most notable in the children who made the switch at a younger age, the researchers reported, noting that “early initiation … is crucial for patients with IOPD.”
The researchers believe these findings emphasize “the critical importance of early treatment initiation for IOPD with [Nexviazyme].” However, the team noted that “further research and long-term large-scale monitoring are needed to elucidate the comparative efficacy, safety, and optimal timing of [Nexviazyme] treatment initiation in patients with IOPD.”
The study, “Efficacy of transitioning from alglucosidase alfa to avalglucosidase alfa in infantile-onset Pompe disease: A single-center cohort analysis,” was published in the journal Genetics in Medicine. It was partially sponsored by Sanofi, which markets both Lumizyme and Nexviazyme.
Both of these therapies are approved for use in U.S. patients, but Nexviazyme is only indicated for individuals with late-onset Pompe and not IOPD. In the U.S., Lumizyme is approved to treat all Pompe disease types.
Nexviazyme approved for IOPD in Europe, Taiwan, though not in US
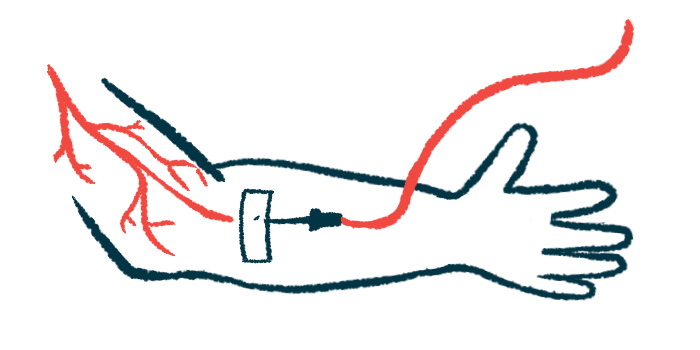
Individuals with Pompe disease lack enough functional acid alpha-glucosidase (GAA), the enzyme that’s needed to break down a large sugar molecule called glycogen. Consequently, glycogen toxically accumulates and causes damage, especially in muscles.
Standard of care treatment for Pompe patients involves enzyme replacement therapy (ERT), in which a version of the deficient GAA enzyme is provided via regular infusions into the bloodstream. ERT is used to treat both late-onset Pompe disease and IOPD. However, achieving adequate disease control for IOPD patients can be more challenging, because it’s a relatively more severe form of the condition, in which natural GAA activity is lower.
Myozyme is an ERT that’s approved in many countries for treating both forms of Pompe. The recommended dose is 20 mg/kg every other week, but clinical studies have suggested that higher doses might lead to better clinical outcomes in IOPD. Such doses, however, could pose safety concerns like a risk of kidney damage or immune reactions, research has shown.
Nexviazyme, sold as Nexviadyme in Europe, is a next-generation product that works similarly to Myozyme but is designed to achieve more efficient muscle cell delivery. In the U.S., it’s only approved for treating LOPD, but it is cleared for IOPD in the European Union and other regions, including in Taiwan.
In this study, scientists in Taiwan described clinical outcomes for nine IOPD patients who had started on Myozyme shortly after birth, but later transitioned to Nexviazyme because of inadequate responses or clinical deterioration.
The children had started on Myozyme at a median age of 2 weeks old. By the time of the switch, all had been receiving Myozyme at higher than recommended doses, with six receiving double and three receiving four times the labeled dose.
As of December 2023, the children had been on Nexviazyme for at least a year, and a median of 4.9 years. All ultimately received the recommended dose of 40 mg/kg given every other week.
Myozyme sold as Lumizyme in US, where it’s approved for all Pompe types
Overall, the results showed improvements in Pompe disease biomarkers after the switch. As of the last follow-up, median blood levels of creatine kinase, a marker of muscle damage, had decreased by 63% and median urine levels of Glc4 — a biomarker of glycogen accumulation — had decreased by 69%.
Functional measures, including those of exercise capacity and lung function, generally reflected stabilizations or improvements after the transition. None of the patients required full-time breathing support with a ventilator or tube feeding after switching.
“Our findings revealed sustained improvements in biomarker levels and improvements or maintenance of clinical function by [Nexviazyme],” the researchers wrote.
Still, outcomes varied. The scientists noted that younger patients and those with better motor function tended to see more obvious improvements.
“Early initiation of [Nexviazyme] is crucial both in naïve patients and when switching therapies,” the scientists wrote.
Our findings revealed sustained improvements in biomarker levels and improvements or maintenance of clinical function by [Nexviazyme].
Three people experienced some form of infusion-related reactions to Nexviazyme, but treatment was able to continue with appropriate management strategies in place. One patient had developed antibodies against Myozyme that persisted after switching to Nexviazyme and which required continuing immune modulation therapy.
High levels of albumin or total proteins in the urine, which can reflect kidney issues, were observed in two patients who had been receiving very high Myozyme doses. This was not observed after transitioning to Nexviazyme.
While the findings demonstrate the possible benefits of Nexviazyme in IOPD, the researchers indicated that additional data from large-scale clinical trials are still needed to better inform the decision-making process for prescribing ERTs in this patient group.
“Further studies are necessary to underscore personalized and tailored treatment approaches that consider individual patient characteristics and disease severity,” the team concluded.