Brain White Matter Abnormalities Found in Pompe Despite Treatment
Study highlights 'urgent need' for new therapies for Pompe patients
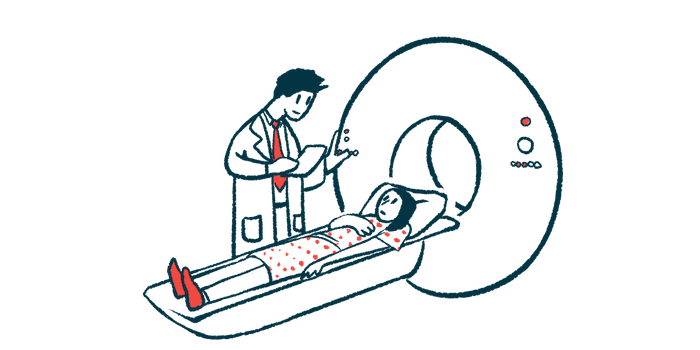
An MRI-based study found that progression of white matter involvement in the brain among patients with infantile-onset Pompe disease (IOPD) occurred at different rates and correlated with cognitive decline — despite ongoing treatment.
White matter abnormalities also were tied to elevated bloodstream levels of the neurofilament light chain (NfL) protein, a sensitive but non-specific biomarker reflecting nerve fiber damage.
These findings support the use of MRI scans and biomarkers such as NfL to monitor neurodegeneration and treatment response in future clinical trials, the researchers noted.
Also, “our study highlights the urgent need to develop therapies targeting neurodegeneration in Pompe disease,” the team wrote.
The MRI study, “Evaluating brain white matter hyperintensity, IQ scores, and plasma neurofilament light chain concentration in early-treated patients with infantile-onset Pompe disease,” was published in the journal Genetics in Medicine.
Investigating brain white matter involvement in IOPD
Classic IOPD, usually diagnosed in a patient’s first few months of life, is marked by progressive muscle weakness, thickening of the heart muscle, and impaired breathing before 6 months of age.
Enzyme replacement therapy (ERT), which provides the GAA enzyme that is missing or dysfunctional in Pompe patients, has significantly improved heart disease outcomes and extended patient survival. With early detection via newborn screening programs, ERT can lead to significant motor improvements and a better quality of life for patients.
With extended survival, and because ERTs cannot access the brain, growing evidence suggests the disease increasingly affects the brain and spinal cord, together known as the central nervous system (CNS).
MRI studies in ERT-treated patients have reported various structural abnormalities in the brain, including changes in white matter — areas of the brain containing nerve fibers coated in myelin, a white, fatty layer that aids in nerve transmission. Moreover, the severity of brain white matter changes seems to increase with age.
Still, few studies have examined these white matter changes in relation to long-term cognitive function and the presence of predictive biomarkers in patients with IOPD.
To learn more, researchers in Taiwan recruited 19 children and adolescents, ages 1.7–19 years, with confirmed IOPD, from the National Taiwan University Hospital. Among the patients, 11 (57.9%) were males. ERT was started for all patients at ages ranging from 5 days to six months (180 days).
At least three brain scans were done during follow-up for 16 patients (84.2%), each of whom was included in further analyses. White matter abnormalities were seen in all of these individuals during follow-up, when scans were performed every one to three years.
Overall, 86 MRI images were scored for white matter involvement. Scores ranged from 0 to 34 points, according to the location and extent of white matter abnormalities and the presence of brain atrophy (shrinkage). Higher scores indicated more white matter involvement.
MRI scores increased with age, with a rate of score increase ranging from about 0.8–2.7 points per year. White matter changes began at a median age of 3.1 years, ranging from 1.5–9.2, and were found in the central white matter before appearing in other areas. Compared with white matter, grey matter was involved to a lesser extent.
Brain atrophy was seen in six participants (37.5%), with two showing cerebrospinal fluid space widening. That fluid, known as CSF, is the protective liquid around the brain and spinal cord.
The individual with the highest MRI score of 30 had brain atrophy at 11.4 years, followed by grey matter involvement, then further atrophy at 14.4 years.
Our study highlights the urgent need to develop therapies targeting neurodegeneration in Pompe disease
IQ scores at the first examination were available for 11 patients, ages 3.6–9.6 years, with a median score of 80 and ranging from low to high average (69–117). The most recent median IQ score, recorded at ages 8.5–13.5 years, was 73 (range: 61–118).
Lower IQ scores significantly correlated with the most recent higher MRI scores, as did worse cognitive scores for perceptual reasoning and processing speed, as assessed by the Wechsler Intelligence Scale for Children.
Finally, significantly higher levels of NfL were found in the bloodstream of 17 patients, as compared with 15 age- and sex-matched healthy controls (median 9.29 vs. 3.97 picograms per mL of blood). NfL concentration between patients appeared to vary widely, with eight individuals showing normal NfL levels and relatively low MRI scores. Regardless, higher blood NfL levels strongly correlated with higher MRI scores.
“[White matter] involvement occurred and progressed in all patients with IOPD at different rates, with a correlation to [blood] NfL levels and decline in cognitive function,” the researchers wrote.
Based on these findings, “further large-scale and longitudinal studies are warranted,” the team said.
Overall, the study showed that “neuroimaging quantification tools and plasma NfL concentration may be a promising biomarker for monitoring CNS progression and patient response to treatment in future trials,” they concluded.