Mitochondria dysfunction linked to cardiomyopathy in Pompe patients
Targeting cellular powerhouses may be novel therapeutic strategy: Study
Mitochondria dysfunction is linked to hypertrophic cardiomyopathy — when the heart becomes enlarged and cannot pump blood efficiently — in people with Pompe disease, according to a new study from China.
The disease-causing mechanisms were explored in a patient-derived heart cell model with characteristics of Pompe disease, including low levels of the acid alpha-glucosidase (GAA) enzyme and accumulation of glycogen.
These effects were partially rescued by supplementing cells with an engineered form of GAA, the approach used in enzyme replacement therapy.
“Targeting the [mitochondria] may therefore serve as a novel candidate adjuvant therapeutic strategy in future [Pompe disease] clinical practice,” the researchers wrote.
The study, “Mitochondrial dysfunction is associated with hypertrophic cardiomyopathy in Pompe disease-specific induced pluripotent stem cell-derived cardiomyocytes,” was published in the journal Cell Proliferation.
Study used stem cells derived from 5-month-old child with IOPD
Pompe is caused by mutations in the GAA gene that lead to a deficiency of the GAA enzyme, which breaks down glycogen — a sugar molecule — into glucose that cells can use to produce energy.
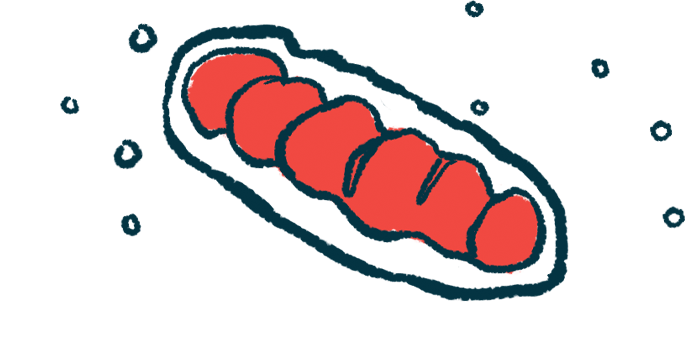
As a result, glycogen accumulates inside lysosomes — cellular compartments where enzymes break down large molecules – in several tissues, including heart muscle cells known as cardiomyocytes. This buildup of glycogen leads to dysfunction among mitochondria, the cellular powerhouses, disrupting the production of energy required for muscle contraction.
It’s unknown, however, “whether mitochondrial dysfunction precedes the development of heart failure,” according to the researchers.
Scientists also don’t know if such impairments drive the transition from compensated cardiac hypertrophy to heart failure in individuals with infantile-onset Pompe disease (IOPD). Patients with IOPD usually have less than 1% of normal GAA enzyme activity.
In this study, cardiomyocytes were generated from induced pluripotent stem cells (iPSCs) derived from a 5-month-old child with IOPD. iPSCs result from fully matured cells that are reprogrammed back to a stem-cell-like state, where they can give rise to nearly every type of human cell. iPSCs from the child’s mother were used as a control.
The child had two mutations, each in one of the two copies of the GAA gene. One was a c.1822C>T, p.R608X mutation inherited from the father and the other was a c.2662G>T, p.E888X mutation inherited from the mother.
Markedly low GAA enzyme levels were found in the child’s blood relative to the normal range — 2.1 vs. 24.8–93.3 nanomol/(g min) — and the infant also was determined to have heart hypertrophy.
The iPSCs were successfully differentiated into cardiomyocytes, confirmed by the expression of cardiac troponin T, a marker of heart muscle. Patient-derived cardiomyocytes were significantly enlarged, as estimated by comparing their average cell surface area with that of control cells. They also had higher activity of genes associated with heart enlargement, including those that encode the markers ANP, BNP, and MHY7.
Mitochondrial defects in the patient’s cardiomyocytes included a significant reduction in function and energy production, along with high levels of reactive oxygen species — potentially toxic molecules due to oxidative damage. Also, there were less mitochondria in heart muscle cells from the child.
Findings support new theory on mitochondrial dysfunction links in IOPD
Further analysis revealed the mechanisms underlying mitochondrial dysfunction. Particularly, there was a reduction in gene activity coding for markers of mitochondrial fusion (MFN1 and MFN2) and mitophagy (PARKIN and PINK1) in the cells derived from the patient, compared with control cells. The fission process was not affected.
Mitochondrial dynamics are characterized by fusion, in which two mitochondria merge, and fission, which refers to their split in two. Mitophagy is a mechanism by which dysfunctional or damaged mitochondria are degraded.
The results also showed low levels of the Sdha protein, a component of one of the mitochondrial protein complexes (complex II) involved in producing energy, in patient-derived heart cells compared with controls.
Mitochondrial defects were eased by supplementing the patient-derived cells with rhGAA, including a significant increase in mitochondrial fusion, mitophagy, and in Sdha levels. The number of mitochondria was markedly increased with rhGAA.
It is vital to explore the mechanisms linking lysosomal and mitochondrial dysfunction that may illuminate the development of novel therapeutic strategies for [Pompe disease].
Heart cell disease also was partially reversed, including less lysosomal glycogen accumulation, lower activity of genes implicated in cardiac hypertrophy, and an increase in mitochondrial energy production. Levels of reactive oxygen species were lowered with treatment.
“Our discoveries support the newly proposed theory that mitochondria dysfunction is associated with hypertrophic cardiomyopathy in IOPD,” the researchers concluded.
Considering that lysosomes play a crucial role in mitophagy, their dysfunction due to accumulated glycogen may impair the clearance of damaged mitochondria, leading to defects in patient-derived cardiomyocytes.
“Therefore, it is vital to explore the mechanisms linking lysosomal and mitochondrial dysfunction that may illuminate the development of novel therapeutic strategies for [Pompe disease],” the researchers added.