Nexviazyme benefits in 3 Japanese Pompe patients match global trials
Gains in lung, motor function similar to that of study populations: Analysis

The benefits seen with Nexviazyme (avalglucosidase alfa) treatment in three people in Japan with Pompe disease matched those found among the overall patient population of two global clinical trials, a new case series analysis by researchers in that country has found.
This trio of Japanese patients — two children with infantile-onset Pompe disease, known as IOPD, and one older man with late-onset Pompe, called LOPD — saw improvements in both lung and motor function, the data showed. Further, no new safety issues were seen with treatment.
These findings are important, according to the researchers, because “individual results of this case series suggest that responses to [Nexviazyme] in Japanese patients with LOPD and IOPD are representative of those seen in [the] overall trial populations.”
While this study was small, it showed that the approved therapy has similar effectiveness and safety in patients in Japan as it did in participants in clinical trials worldwide, the team noted.
The study, “Efficacy and safety of avalglucosidase alfa in Japanese patients with late-onset and infantile-onset Pompe diseases: A case series from clinical trials,” was published in the journal Molecular Genetics and Metabolism Reports. The work was funded by Sanofi, which markets the therapy; three of the nine authors are employees of the company.
Researchers note genetic difference between Japanese, Western patients
In people with Pompe, inherited mutations cause a deficiency in the activity of acid alpha-glucosidase, or GAA, an enzyme needed to break down a complex sugar molecule called glycogen. Without this activity, glycogen accumulates to toxic levels in body tissues, especially in muscle.
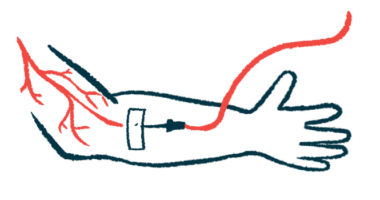
Nexviazyme, which was developed by Sanofi, is an enzyme replacement therapy, or ERT, that provides a lab-made source of GAA. It is intended to deliver the enzyme to muscle cells, and to lower glycogen levels more effectively than Lumizyme (alglucosidase alfa), an older ERT also developed by Sanofi.
Given via intravenous, or into-the-vein, infusion every two weeks, Nexviazyme is approved in the U.S. for people with LOPD, ages 1 and older. In Europe and Japan, the therapy is approved for both late- and infantile-onset forms of Pompe.
Data from the Phase 3 COMET trial (NCT02782741) and the Phase 2 Mini-COMET study (NCT03019406) supported Nexviazyme’s various approvals. COMET compared Nexviazyme versus Lumizyme in 100 patients with LOPD, ages 3 and older, who had never been on ERT. Mini-COMET enrolled 22 children with IOPD who had previously failed to respond to Lumizyme.
In this report, a team led by scientists at the National Center of Neurology and Psychiatry in Japan, and involving the Sanofi researchers, described the outcomes of three Japanese patients: the older man, who participated in COMET, and the two children, both of whom were enrolled in Mini-COMET.
The work was important, according to the researchers, because the genetic alteration most common in people with Pompe in Japan “[differs] from the most frequently seen … gene variant in [Pompe] patients from Western and other Asian countries.” The team also noted differences seen in the age of LOPD onset.
“A known genetic difference, combined with probable region-specific lifestyle differences, suggests the need to separately verify the efficacy and safety of [Nexviazyme] in Japanese patients enrolled in clinical trials,” the researchers wrote.
Gains with Nexviazyme seen for Japanese man, 60, and 2 children
The first patient described in the case series was a 60-year-old man with LOPD, who, before the COMET trial, had muscle weakness affecting his breathing and ability to stand up.
During the trial, which spanned 49 weeks or about one year, the man’s lung function improved slightly compared with the overall trial population. Still, in the six-minute walking test (6MWT) for exercise capacity, his walking distance initially declined but improved beyond the overall population at 49 weeks.
His total scores in the quick motor function test, known as QMFT, improved in parallel with those of other trial participants. Changes in the levels of biomarkers, such as creatine kinase for muscle damage and urinary Hex4 for glycogen storage, also were similar. Overall, Nexviazyme was well tolerated in this patient, according to the researchers.
The second case detailed involved a boy with IOPD with a family history of the disease who showed early signs of heart problems and muscle weakness. These symptoms had required support for movement and breathing by age 6. Mild motor and speech developmental delays were also noted. The child was prescribed Lumizyme soon after diagnosis, but due to clinical decline, he joined Mini-COMET.
Improvements in motor function, as indicated by gross motor function measure-88 and QMFT, were observed over six months of treatment and matched the mean values of the overall trial population. While the patient’s heart alterations eased, his eyelid drooping did not. Reductions in creatine kinase exceeded those seen in the trial population, while changes in urinary Hex4 were similar.
Starting at age 5, hearing impairment had been noted during episodes of worsening middle ear infections, which are known as otitis media. However, the child’s condition eased with Nexviazyme, and no hearing aid was required. No major safety issues were reported with this patient.
We conclude that [Nexviazyme] provides an efficacy and safety profile in Japanese patients representative of that of the overall populations from key international trials.
The third patient was a girl who first showed symptoms at 6.5 months of age, with poor weight gain and delayed neck control. At her IOPD diagnosis, at 7.2 months old, she had an enlarged heart and liver. She began Lumizyme treatment at 10 months. By age 10, however, she experienced a decline while on Lumizyme and enrolled in Mini-COMET. Unlike the boy, her muscle weakness was mild, and she could walk without assistance.
After six months in Mini-COMET, the girl experienced improvements in motor function that matched the mean values for the overall population. While there were few changes in heart measures, her lung function and 6MWT results improved. Changes in creatine kinase and urinary Hex4 were similar to those in the overall population.
The scientists noted that, “importantly, no new or unique safety signals were detected among Japanese patients with LOPD or IOPD” with this treatment.
“We conclude that [Nexviazyme] provides an efficacy and safety profile in Japanese patients representative of that of the overall populations from key international trials,” the team wrote.