Infusion-associated reactions to ERT mostly mild, nonallergic in Pompe
Defined retreatment strategies needed in the event of discontinuation, researchers said
Hypersensitive reactions to infusions of enzyme replacement therapies (ERT) to treat late-onset Pompe disease (LOPD) were primarily mild and nonallergic, a small study reported.
Many reactions were reported after a year of well tolerated ERT and most of them occurred in women, data showed.
After the reactions, the ERT was safely reintroduced using modified treatment regimens and a desensitization protocol, starting with low doses until the cumulative therapeutic dose was reached and tolerated.
Further studies are needed to investigate the biological mechanisms underlying these reactions to identify predictive factors and define ERT re-treatment strategies, the researchers recommended in “Hypersensitivity infusion-associated reactions induced by enzyme replacement therapy in a cohort of patients with late-onset Pompe disease: An experience from the French Pompe Registry,” which was published in Molecular Genetics and Metabolism.
Pompe disease is marked by an inherited deficiency in acid alpha-glucosidase (GAA), an enzyme that breaks down the energy-storage sugar molecule glycogen. Insufficient GAA activity results in glycogen building up to toxic levels, especially in muscle cells, leading to the onset of symptoms.
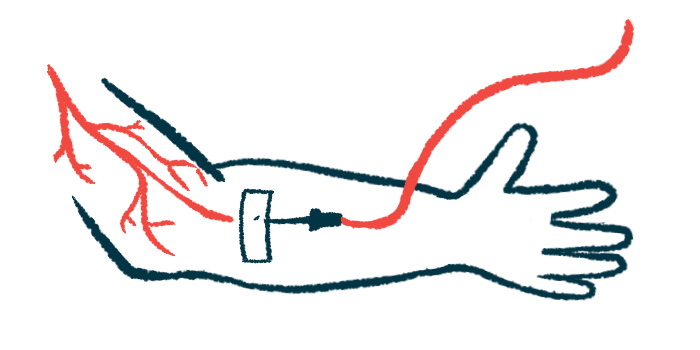
ERTs are the only approved Pompe treatment that provide a lab-made source of GAA to aid glycogen breakdown and slow muscle damage progression. The treatment is administered through regular infusions into a vein every other week, lasting 4-5 hours.
Infusion-associated reactions (IARs) — hypersensitivity reactions that develop during or shortly after an infusion — have been reported in up to 40% of LOPD patients. Many have been linked to drug hypersensitivity reactions (DHRs), which can lead to the treatment being discontinued.
Common IAR symptoms include injection-site swelling and itch, nausea, increased blood pressure, high body temperature, flushing, chills, headache, and in some cases, anaphylaxis, a severe allergic reaction.
Reactions to ERT infusions
However, “there are currently no established guidelines concerning ERT discontinuation or reintroduction after hypersensitivity IAR (or DHR) in Pompe disease,” wrote the researchers who examined hypersensitivity IARs and their management in LOPD patients in France and investigated approaches to restarting an ERT after a reaction.
Data were collected from 15 LOPD patients (12 women) treated with ERT who had at least one IAR episode, with six reporting more than one. Most patients (73.3%) had their first IAR (or DHR) episode after the first year of treatment and three (20%) after more than two years.
Eighteen (64.3%) skin-only reactions (Grade 1) occurred and there were nine (32.1%) reactions with skin involvement with other non-life-threatening signs (Grade 2). One (3.6%) life-threatening symptom (Grade 3) reaction happened.
There were 16 (57.1%) reactions involving injection-site redness, eight (28.6%) chest and/or throat tightness reactions, four (14.3) instances of shortness of breath, chills and/or cold sweats, and facial swelling, three (10.7%) instances of low oxygen, and two (7.1%) of high blood pressure.
Only two hypersensitivity cases (13.3%) were mediated by a type of antibody called immunoglobin E (IgE) against GAA, a sign of an allergic response to treatment. All other reactions were non-IgE related (nonallergic).
ERT was stopped in 10 cases (66.7%), five of whom continued with other medications, including pre-medications such as antihistamines and corticosteroids. Motor and lung function worsened after the ERT was discontinued. It was reintroduced in nine patients with a median time from discontinuation to re-treatment of 15.1 months.
Before ERT, six of the nine had pre-medication combined with a desensitization protocol, defined as a slow increase from a low to a tolerated therapeutic dose. Two patients started with a low dose and slow infusion rates for the first three ERT re-treatments, while one just took pre-medications. Reintroducing the ERT was safe in all patients, regardless of IgE-mediated drug reactions.
“ERT-induced DHR can be safely and effectively managed with a modified regimen or desensitization protocol in LOPD patients,” the researchers wrote. “Further studies are required to investigate the biological mechanisms of DHR, to identify predictive factors, and to further define ERT re-challenge protocols.”







