FAQs about Nexviazyme
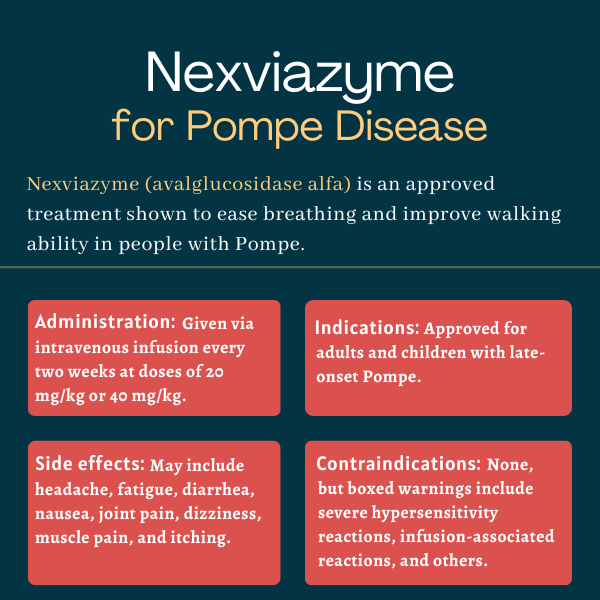
The U.S. Food and Drug Administration approved Nexviazyme in 2021 to treat late-onset Pompe disease in patients ages 1 and older.
Nexviazyme has not been well-studied in pregnant individuals. It is recommended that the therapy’s use during pregnancy be tailored based on the needs of the individual, in consultation with the patient’s healthcare team.
There is no direct evidence reported of an interaction between alcohol and Nexviazyme. Patients are, however, advised to talk to their healthcare providers about the use of alcohol or other substances while taking Nexviazyme.
Some patients have seen benefits in just over three months of treatment. In the COMET Phase 3 clinical trial that compared Nexviazyme against Lumizyme in people with late-onset Pompe disease, improvements in lung function with Nexviazyme were noted after about 13 weeks. There is, however, no standard timeline for Nexviazyme’s benefits, as each person may respond differently to the medication.
Neither hair loss nor weight gain has been reported as common side effects of Nexviazyme. People who experience unexpected effects after starting a new therapy are advised to seek the advice of their healthcare team.
 Fact-checked by
Fact-checked by