Q&A with Sanofi: Nexviazyme Safely Aids Muscle Strength in LOPD
Newly approved Nexviazyme (avalglucosidase alfa) is a next-generation, alternative enzyme replacement therapy for late-onset Pompe disease patients starting at age 1.
In clinical trials that supported the Aug. 6 approval by the U.S. Food and Drug Administration (FDA), meaningful improvements in respiratory muscle strength and mobility were evident in patients given Nexviazyme relative to those on Lumizyme (alglucosidase alfa), the disease’s only other approved enzyme replacement therapy (ERT). Sanofi developed and markets both treatments.
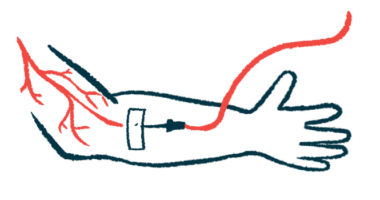
Nexviazyme is designed to more effectively deliver the enzyme needed to break down glycogen to muscle cells and to clear this complex sugar molecule from those cells, preventing its damaging accumulation. Disease-causing GAA mutations affect the acid alpha-glucosidase (GAA) enzyme normally produced by this gene.
Specifically, Nexviazyme binds more strongly than Lumizyme to mannose-6-phosphate (M6P) receptors that reside on a target cell’s surface, so its replacement enzyme is better able to enter to cells, a process called enzyme uptake.
Karin Knobe, MD, PhD, head of Rare Diseases and Rare Blood Disorders Clinical Development at Sanofi, responded to questions asked by Pompe Disease News about Nexviazyme in an email exchange.
Here is our Q&A, with ellipses marking spots where highly scientific points, like trial p-values, were removed:
Question: Nexviazyme is an advance on Lumizyme, in that it is designed to improve GAA enzyme uptake and glycogen clearance in target skeletal and heart muscles. Like Lumizyme, it does so by working through mannose-6-phosphate receptors, but is reported to do so with greater specificity.
Please describe what is meant by greater specificity in receptor binding with Nexviazyme, and how this specificity was evident in key primary and secondary efficacy findings in the COMET Phase 3 trial, and the Mini-COMET Phase 2 study.
Knobe: Nexviazyme is specifically designed to target the M6P receptor, which plays a key role in the transport of the GAA enzyme to clear glycogen. Nexviazyme has an approximate 15-fold increase in M6P content compared to Lumizyme (alglucosidase alfa). This enhanced binding affinity aims to increase cellular enzyme uptake and enhance glycogen clearance in muscle cells.
In the Phase 3 COMET trial [NCT02782741], Nexviazyme showed improvement in critical manifestations of late-onset Pompe disease. The trial successfully met its primary objective, evaluating the change in respiratory muscle function using forced vital capacity (FVC) percent-predicted in the upright position vs. baseline [trial’s start]. When compared to baseline, patients treated with Nexviazyme had a 2.9-point improvement … in FVC percent-predicted at Week 49.
Additionally, patients treated with Nexviazyme had a 2.4-point greater improvement in FVC percent-predicted compared to patients treated with alglucosidase alfa … a numerical improvement in respiratory function that met the study-designed primary endpoint of non-inferiority … Statistical superiority of Nexviazyme over alglucosidase alfa was not shown in the study.
A key secondary endpoint in the Phase 3 COMET trial measured functional endurance with the 6-minute walk test (6MWT). When compared to baseline, patients treated with Nexviazyme walked 32.2 meters farther … at Week 49. Additionally, patients treated with Nexviazyme walked 30 meters farther … than patients treated with alglucosidase alfa at Week 49. Per the hierarchy of the study protocol, formal statistical testing for all secondary endpoints was not conducted.
Question: What are these findings expected to mean, in everyday life terms, to children and adults with late-onset Pompe disease?
Knobe: Late-onset Pompe disease (LOPD) is a progressive and debilitating condition and people living with LOPD experience impairment in respiratory function and mobility, which impacts their ability to breathe and move. As the disease progresses, people with LOPD may require mechanical ventilation to help with breathing or a wheelchair to assist with mobility.
Historically, there has only been one approved treatment option and people on treatment may progress on therapy, often experiencing a decline in muscle function over time.
Nexviazyme has demonstrated improvements for people living with LOPD. In the pivotal Phase 3 COMET trial, Nexviazyme showed improvements in respiratory function and walking distance measures in people with LOPD and established its safety profile.
Question: Better respiratory strength and walking distance were the two key efficacy gains with Nexviazyme relative to Lumizyme in the COMET study, but better physical and, particularly, mental health-related quality of life were also reported by enrolled adults.
In your opinion, why did Nexviazyme lead to a 0.77-point rise in physical health and a 2.12-point increase in mental health on these SF-12 tests? Given that both are twice-monthly infusion treatments, what might patients be saying through these scores?
Knobe: SF-12 is patient-reported assessment of health-related quality of life as it relates to their physical and mental health.
The results seen in the COMET study from 49 weeks of treatment with avalglucosidase alfa [Nexviazyme] during the primary analysis period indicate that, on average, patients are reporting improvements in their physical and mental health-related quality of life compared to the start of treatment. This is consistent with previously published data that demonstrated that improvements in clinical outcomes correlate with improvements in patient reported outcomes.
Question: Safety was shown throughout the trials, with a side effects profile similar to Lumizyme: fatigue, headache, nausea, and rash or itching. Two COMET patients had serious adverse events, as did three on Lumizyme.
Please discuss the nature of these serious and common side effects, particularly noting if the serious events were anaphylactic or allergic reactions — possibly implying antibody development to the treatment — or immune-mediated reactions.
Knobe: In the double-blind, active-controlled period of the COMET study, one patient treated with avalglucosidase alfa experienced a serious adverse reaction, and three patients treated with alglucosidase alfa [Lumizyme] experienced serious adverse reactions.
The one patient who experienced a serious adverse reaction during treatment with avalglucosidase alfa reported shortness of breath, which was determined to be treatment-related. This resolved and the patient continued treatment in the study.
Overall, the occurrence of infusion-associated and hypersensitivity reactions was higher in patients with high anti-drug antibodies in clinical trials with avalglucosidase alfa. Fewer patients randomized to avalglucosidase alfa in the COMET study reported high antibody titers compared to those randomized to alglucosidase alfa.
Question: Are Nexviazyme’s infusion times and rates also similar to Lumizyme?
Knobe: Both Nexviazyme and Lumizyme are administered intravenously [into the vein] every two weeks incrementally as determined by the patient’s response and comfort.
Question: COMET enrolled late-onset patients starting at 3 years old. Were you surprised by a late-onset approval for patients starting at age 1, or was this somewhat expected, as Sanofi’s application request was based on results in both infantile- and late-onset Pompe?
Knobe: Our clinical development program for Nexviazyme evaluated the therapy in the full spectrum of Pompe disease, including both late-onset Pompe disease in adults and pediatric patients, as well as infantile-onset Pompe disease.
Question: Is a Phase 3 trial in infantile-onset Pompe disease being planned for Nexviazyme, or are approval discussions underway or intended based on Mini-COMET findings?
Knobe: The Phase 2 Mini-COMET study [NCT03019406] evaluated the safety of Nexviazyme, and efficacy measures were exploratory.
To gain an infantile-onset Pompe disease (IOPD) indication, additional data will be required. As planned, the Phase 3 Baby-COMET study [NCT04910776] in naïve IOPD [patients less than] 6 months old is currently enrolling. [This open-label trial is recruiting up to 16 infants at a site listed in Italy.]
Lumizyme is FDA-approved and available for IOPD.
Question: Are further trials planned for Nexviazyme in any Pompe patient groups?
Knobe: Our clinical development program for Nexviazyme is evaluating the therapy in the full spectrum of Pompe disease, including both late-onset Pompe disease in adults and pediatric patients, and infantile-onset Pompe disease, as well as both naïve and previously treated patients. Several clinical trials are ongoing.
Our Phase 3 COMET trial included an open-label extension evaluating forced vital capacity and 6-minute walk test in those patients who switched from alglucosidase alfa to Nexviazyme at 49 weeks, which is ongoing. Full results will be presented at a future medical congress.
NEO-EXT [NCT02032524], the long-term open-label extension study of patients previously treated with alglucosidase alfa from the NEO1 trial, which evaluated the safety, tolerability, pharmacokinetics, pharmacodynamics, and exploratory efficacy of Nexviazyme in patients with LOPD, is also ongoing. [Pharmacokinetics refers to the movement of a drug into, through, and out of the body; pharmacodynamics refers to its effects on the body].
Question: Where, in your opinion, does approval stand for Nexviazyme with the European Union, and why does Sanofi consider it important to have the European Medicines Agency recognize it as a “new active substance”?
Knobe: The Committee for Medicinal Products for Human Use (CHMP) previously adopted a positive opinion for avalglucosidase alfa, recommending the granting of a marketing authorization [in the EU] for the treatment of Pompe disease.
While we are pleased the committee recognized the value of approving avalglucosidase alfa for the global Pompe community, we are disappointed with the CHMP opinion regarding the new active substance designation. We firmly believe avalglucosidase alfa qualifies as a new active substance (NAS) based on the product characteristics and robust clinical data. As a result, we have requested a re-examination of the CHMP opinion in relation to the NAS conclusion.
Question: What services are available to Pompe patients and their families through Sanofi’s CareConnectPSS Patient Support Services?
Knobe: Sanofi’s CareConnectPSS patient support program (1-800-745-4447, Opt. 3) provides personalized support for people and their families impacted by Pompe disease, including eligible patients transitioning to Nexviazyme. This includes one-on-one assistance with insurance, disease and treatment education, and treatment logistics.
Question: What other work is ongoing or planned at Sanofi into Pompe disease, in terms of new ERTs or other potential therapies? Is work underway on a treatment aiming to address the disease’s root cause?
Knobe: Our internal research teams continue to learn from our 20 years of experience and to publish their findings in an effort to advance care for people living with Pompe disease.
An important aspect of that research is understanding the underlying disease. Sanofi Genzyme’s global Pompe Registry, one of multiple Global Rare Disease registries, has followed the natural history and outcomes of people living with Pompe disease for more than a decade. This real-world evidence helps [healthcare providers] better understand patients’ health and informs future research efforts.
To date, the Pompe Registry has resulted in seven publications expanding the understanding around Pompe disease.
Question: Is there anything you would like to add?
Knobe: Due to its rarity and lack of awareness surrounding the symptoms of Pompe disease, many times patients do not receive an accurate diagnosis of Pompe for extended periods of time, leading to a delay in treatment and reduced quality of life. With a progressive condition like Pompe, early diagnosis and treatment initiation is critical.
In addition to treatment options, people living with Pompe disease and their families have a multitude of other needs. We commend the incredible work of healthcare providers and patient advocacy organizations in the U.S. and around the world who work tirelessly to identify and support the individual needs of people impacted by Pompe disease. We deeply appreciate and admire their steadfast commitment and advocacy efforts.